SECOND INTERNAL EXAMINATION
This is an online e-log book to discuss our patient de-identified health data shared after taking his / her / guardian's signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
This E blog also reflects my patient-centered online learning portfolio and your valuable input in the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and coming up with diagnosis and treatment plans. is an online e-log book to discuss our patient's de-identified health data shared after taking his / her / guardians' signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
CASE REPORT
A 65-year-old male patient resident of Choutuppal once a farmer (stopped working 6 years back)
came to the medical OPD with the
PERSONAL HISTORY:-
Appetite - Reduced since 1 year
Diet - Mixed
Bowel and Bladder - Regular
Sleep - inadequate
Addictions - stopped 20 years back, before alcohol and smoking
ALLERGIC HISTORY:-No allergies to any kind of food or medication.
A 65 old male patient, supine decubitus who Is conscious, coherent and cooperative
comfortably seated/lying on the bed, well-oriented to time,
place and person
There is Pallor
No, Icterus, cyanosis, clubbing
generalized lymphadenopathy and no pedal edema
Pulse: Rate, rhythm(regular)character(
peripheral pulsations [Carotid, brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis]- present
no radio radial delay
BP: 120/80 mm Hg measured on Rt Upper arm In supine position
Respiratory Rate:25 CPM; type- Abdomino thoracic
The above-mentioned positive history is in favor of respiratory; GIT and CVS hence I have examined all the systems.
RESPIRATORY SYSTEM:-
INSPECTION:
1. Shape of Chest - normal
2. Trachea position central
3. Apical Impulse - no visible
4. Movements of the chest: Respiratory rate:- 14cpm Type- abdomino thoracic type no accessory muscles involved.
5. Skin over the chest: Any engorged veins, sinuses, subcutaneous nodules, intercostal scars, or intercostal swellings.
6. All the areas appear normal.
PALPITATION:
1. No local rise in Temperature and tenderness
2. All inspector findings confirmed. (Tracheal position, apex beat)
3. Expansion of the chest- equal in all planes
PERCUSSION:
Resonant all over the chest except infraxillary area
AUSCULTATION:
1. Normal breath sounds were heard in all areas except the left infra axillary where there are decreased breath sounds.
PER ABDOMEN:-
INSPECTION:
9 REGIONS
Shape (scaphoid)
No Distention of Abdomen
Flanks- full
Umbilicus- normal
The skin over the abdomen: (smooth)
No engorged veins, visible pulsations, or hernia orifices.
PALPATION:-
Tender in the following areas.
No hepatomegaly and splenomegaly
PERCUSSION:
Normal
AUSCULTATION:
1. Bowel Sounds - heard
CVS:-
INSPECTION:-
Appears normal in shape
Apex beat is not visible
PALPITATION:
1- All inspector findings were confirmed.
2-Trachea is central.
3-Apex Beat - diffuse
No palpable murmurs (thrills)
AUSCULTATION:-
S 1; S 2 heard in all the areas
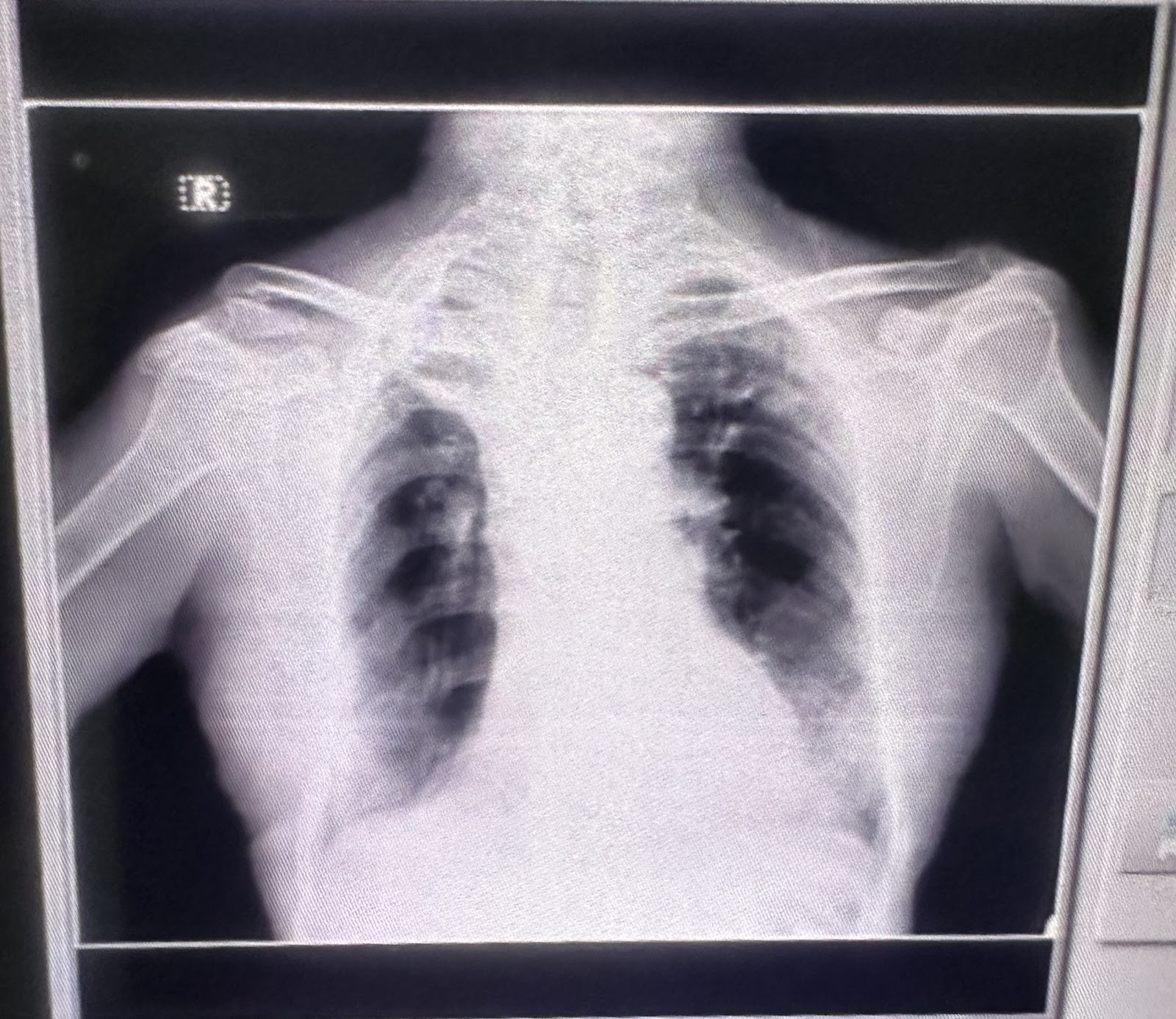
INVESTIGATIONS:-
29-11-2022
30-11-2022
PROVISIONAL DIAGNOSIS:-
Pain abdomen under evaluation
Heart failure with mid range reduced ejection fraction (52%)
with Anemia under evaluation with Chronic kidney disease
with a history of Pulmonary TB- 25 years back
TREATMENT:
Head end elevation up to 30 degrees
supplementation if spo2
<90%
MONITOR 4- hrly
NEB - SALBUTAMOL 4 hrly
FEVER CHART 4 th hrly
InJ LASIX 4O mg
DAY 1 FOLLOW-UP:-
SUBJECTIVE:
4 Episodes of loose stools
OBJECTIVE:
Pt is c/c/c
Afebrile
BP- 120/80mmHg
PR-76bpm
RR-20cpm
SpO2-98%
GRBS-98mg/dL
CVS-S1S2+
RS-BAE+
PA-soft, tenderness at Rt hypogastrium and left lumbar region
CNS-NFD
I/O- 1000/800ml
ASSESSMENT:
Pain abdomen with COR PULMONALE HEART FAILURE WITH MID RANGE EJECTION FRACTION with H/O PULMONARY KOCHS- 25 years back with ANEMIA under evaluation with AKI on PCKD
PLAN:
1. HEAD END ELEVATION UPTO 30 degrees
2. INJ AUGMENTIN 1.2g IV/STAT
3. INJ PANTOP 40mg/IV/BD
4. NEBULIZATION WITH SALBUTAMOL 4 the hourly
5. INJ LASIX 20mg/IV/BD
6. INJ SPORLAC- DS po/TID
7. ORS sachets




























Comments
Post a Comment