A 85 year old male patient came with the complaints of shortness of breath since 2 days
This is an online e-log book to discuss our patient's de-identified health data shared after taking his / her / guardian's signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
This E blog also reflects my patient-centered online learning portfolio and your valuable input in the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and coming up with diagnosis and treatment plans. is an online e-log book to discuss our patient's de-identified health data shared after taking his / her / guardians' signed informed consent. Here we discuss our individual patients' problems through a series of inputs from the available global online community of experts with an aim to solve those patients' clinical problems with collective current best evidence-based information.
A 85 year old male patient came with the complaints of shortness of breath since 2 days
Complaints of shortness of breath since 2 days
morning.
Complaints of bloating since yesterday
Complaints of decreased urine output since Morning.
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 2 days back then developed difficulty in breathing which is insidious in onset gradually progressive
H/O PND, orthopnea present
H/o pedal edema present
H/o abdominal distension present
No H/o fever with pain, sore throat
No H/o involuntary movement
NoH/o skin manifestations like rash, nodules
No H/o Recurrent respiratory infection
Syncope
No H/o Hemoptysis
No History of chest pain ; palpitations; loss of consciousness
PAST HISTORY:-
No similar complaints in the past
Not a known case of DM ;HTN; CAD; CVA ; Thyroid ; TB ; asthma epilepsy .
Personal history:-
Diet - mixed
Appetite- normal
Sleep - adequate
Micturition:- decreased
Addictions :- chronic smoker of chutta which he stopped 6 years back due to complaint of hemoptysis which was investigated?? And found no pathology !
Allergic history:- No history of any kind of allergies for food/drugs
Family history:- no significant family history
GENERAL EXAMINATION:-
At the time of examination :- 7/9/23
PATIENT IS CONSCIOUS COHERENT AND CO OPERATIVE
NO PALLOR ; ICTERUS; CLUBBING; CYANOSIS; ; LYMPHADENOPATHY
EDEMA PRESENT
TEMPERATURE:- AFEBRILE
PR:110bpm
BP:140/80mmHg
RR:32cpm
SYSTEMIC EXAMINATION:-
RESPIRATORY SYSTEM:-
RESPIRATORY SYSTEM:-
INSPECTION:- Chest appears symmetric
No Dilated veins, scars, sinuses
INSPECTION:
1. Shape of Chest - normal
2. Trachea position central
3. Apical Impulse - no visible
4. Movements of the chest: Respiratory rate:- 34cpm .
5. Skin over the chest: NO engorged veins, sinuses, subcutaneous nodules, intercostal scars, or intercostal swellings.
6. All the areas appear normal.
PALPATION:
1. No local rise in Temperature and tenderness
2. All inspector findings confirmed. (Tracheal position, apex beat)
3. Expansion of the chest- equal in all planes
PERCUSSION:
Resonant all over the chest except infraxillary area and infrascapular area .
AUSCULTATION:
1. Normal breath sounds were heard in all areas except IAA AND ISA .
Crepts are heard in IAA And ISA .
CVS EXAMINATION:-
S1 S 2 heard ; NO MURMURS
PER ABDOMEN:-
no tenderness
no palpable organs
bowel sounds - present
CNS EXAMINATION:-
The patient is conscious.
No focal deformities.
cranial nerves - intact
sensory system - intact
motor system - intact
INVESTIGATIONS:-
On the day of admission 6/9/23:-
Serology:- NEGATIVE
RBS - 134 mg/dl
B.urea - 53 mg/dl
S.Cr - 2.4 mg/dl
Na - 140 mEq/L
K - 4.3mEq/L
Cl- 103mEq/L
CUE -
Albumin ++++
Sugar - Nil
Pus cells - 8-9 cells
Epi cells - 2-3 cells
RBC :- 10-12 cells
Hb- 13.0
TLC - 18,000
MCV - 92
MCH - 30.7
МCHC - 34.0
PLT - 2.56 LAKHS
7/9/23 :-
Hb:- 13.5
TLC :- 20,500
PLT :- 2.6 lakhs
ECG ON 6/9/23 :-
On 7/9/23 :-
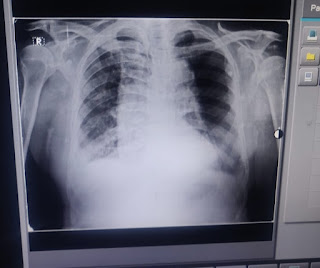
CXR :-
DIAGNOSIS:- ACUTE EXACERBATION OF COPD WITH ACUTE COR PULMONALE WITH DE NOVO DM II AND HTN .
TREATMENT:-
- INJ LASIX 40 mg IV/BD IF SDP >110mmHg
- INJ AUGMENTIN 1.2 gm IV/BD
- Intermittent Bipap
- TAB AZITHROMYCIN 500 mg PO/OD
- INJ HYDROCORT 100 mg IV/TID
- Inj aminophylline 500 mg IV / SOS
- INJ HAI S/C TID ( inform Grbs)
- Salt restriction < 2g / day; fluid restriction < 1.5
- Nebulisation with budecort; mucomist
- Inj N ACETYL CYSTEINE 400mg IV / SOS
- TAB ECOSPIRIN AV 75/10 Po/HS
Date :- 8/7/23
INVESTIGATIONS:- TROP I :- 9,693
Hb :- 13.3
TLC :- 24,500
PLT :- 2.3
Sr CREAT :- 2.9
SOAP NOTES
08-09-2023:
ICU BED1
S:
Bloating of stomach
Shortness of breath grade 3
O:
I/o - 1000/1400 ml
Bp- 140/90 mmhg
Pr - 103 bpm
Rr- 24 cpm
Spo2 - 99% at 4L O2
Grbs - 183
CVS - S1 S2 + No murmurs
RS - BAE+ ,B/l wheeze+ ,crepts+ in Rt IAA and Rt ISA
P/A - Soft and NT
CNS - NFND HMF+
A:
DIAGNOSIS:-
HF with reduced EF(EF=30%) secondary to CAD (NSTEMI )with acute exacerbation of COPD with type 1 Resp Failure with Acute Cor pulmonale with AKI (renal) with denovo DM 2 and HTN
P:
1.Inj Heparin 5000Us/c TID
2.INJ LASIX infusion 10 mg/hr
3.Intermittent Bipap
4.INJ HYDROCORT 100 mg IV/TID
5.Inj aminophylline 500 mg IV / BD
6.INJ HAI S/C TID ( inform Grbs)
7.Inj MgSo4 1gm IV/OD
8.Nebulisation with budecort; mucomist
9.Inj N ACETYL CYSTEINE 400mg IV / BD
10.Tab Ecosprin AV (75/10) PO/HS
11.Tab Met - XL 25 mg PO/OD
12.GRBS 7 point profile









Comments
Post a Comment